At the end of this module, you will:
What is cancer-related fatigue?
Fatigue is when you feel tired, weak or drained. It usually relates to the amount of physical activity you have done. Cancer-related fatigue is different to regular fatigue because it is persistent, debilitating at times, and doesn’t go away with sleep or rest. Some people describe it as all-encompassing mental and physical exhaustion.
Is it common?
Fatigue is the most common symptom reported by people with cancer. In fact, it affects 80 – 100% of cancer patients. Those who experience fatigue agree that it dramatically impacts their everyday functioning, ability to work and enjoyment of life.
A study exploring fatigue for people undergoing cancer treatment found 61% reported fatigue adversely affects their ability to work, 57% said they are unable to enjoy life fully and 61% said fatigue affects their lives more than the pain.
Even though it is common, managing fatigue is an important part of cancer care. This module will provide tips and tools to help you sustain energy and reduce the impacts of fatigue.
Signs and Symptoms
Fatigue affects people with cancer in different ways. Levels of fatigue can also vary depending on your type/stage of cancer, treatment, and pre-existing health conditions.
That said, there are some commonalities in experience. We asked people with cancer to explain what their fatigue feels like:
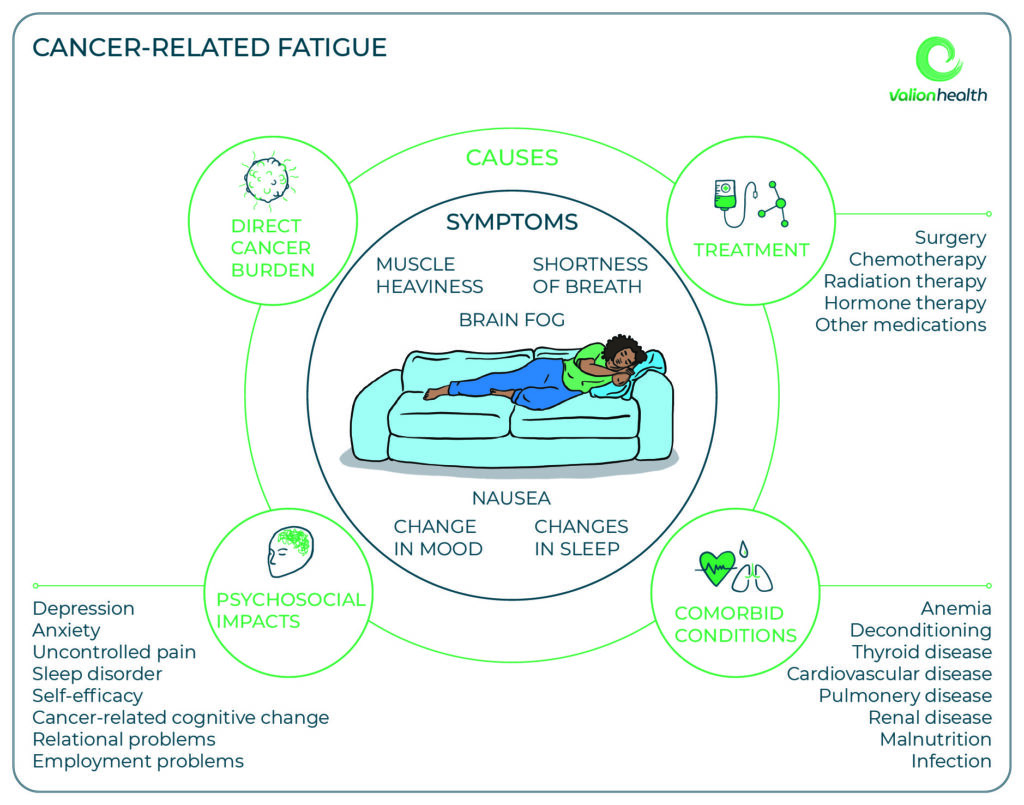
What cause this fatigue??
Contrary to popular belief, fatigue is not just related to the effects of chemotherapy and radiation. There are many factors involved which spread across the direct impact of cancer itself, your specific treatment pathway, psychosocial issues and other health conditions.
Cancer-related fatigue is not as simple as cause and effect! Its multifactorial nature can make it very difficult to treat and address. The best way to tackle fatigue is by identifying causal factors and developing a management plan.
The impact of fatigue
Fatigue is more than a debilitating physical symptom. It can be incredibly distressing and demoralising – especially if you start to compare your previous energy/ activity/ productivity levels with your current levels. It can bring up issues around self-worth and self-identity, as well as activate anxiety, fear and grief.
Understanding your body battery
 |
One way to understand your new fatigue is through the concept of a body battery. Prior to being unwell, you may have had a physical and cognitive battery that fully charged and could run for 12-14 hours. Since being unwell, your battery ‘drains’ faster, especially through intense activities, and hence requires charging more often. |
Two common patterns people fall into
There are two common patterns people with cancer often find themselves in when trying to combat fatigue. We have outlined them below. Both are ineffective and can actually increase fatigue and its impacts. Do you notice these cycles in yourself?
1. Boom and Bust Cycle
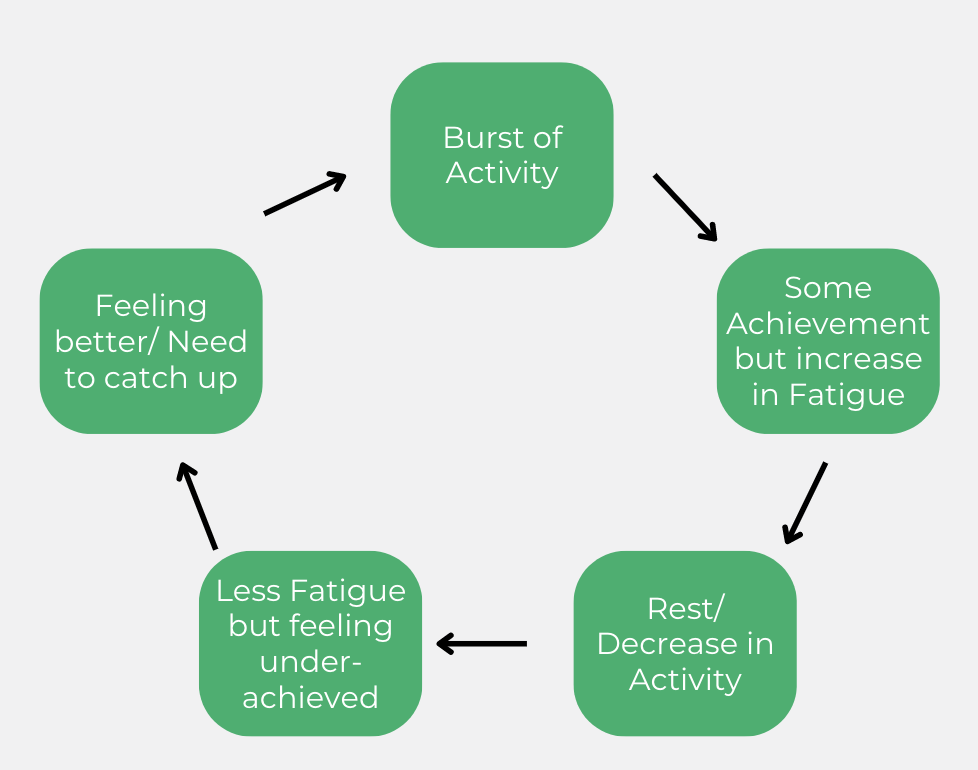
This cycle essentially involves waking up feeling quite energised and wanting to capitalise on this energy by completing a lot of activities. This results in major fatigue and a need to either rest for extended periods, or reduced ability to function for a full day.
2. Continuous Rest
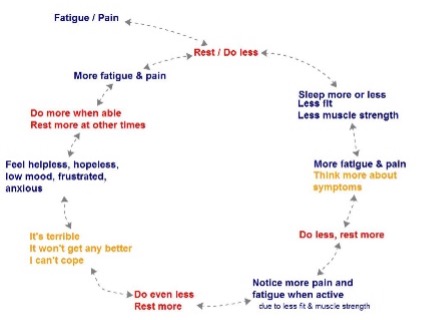
This cycle is usually established over time. It starts with fatigue and/or pain which triggers rest. By resting a lot or reducing activity over time this decreases strength, so that when you are active again you notice further fatigue or pain. As a result, you become disheartened and experience intrusive thoughts which demotivate you from trying further activity.
If you recognise either of these cycles in yourself, bring them up with your clinician, as they are useful in understanding why you may be feeling more fatigued that usual.
Also, don’t panic, there are things you can do to break the cycle! Check out the tips in the following sections.
TIPS: Monitoring your fatigue
The best way to understand your fatigue is by monitoring it alongside your sleep pattern and activity levels. We have provided an explanation and links to template logs/ diaries you can use to help with monitoring.
 |
Fatigue Scale
Having a scale to measure daily fatigue levels is useful in drawing its connection to activity, sleep and treatment undertaken. You can use the simple scale and log developed by Valion Health to record your daily fatigue level. A body scan meditation can help you identify when you may need to stop and take a break rather than waiting until you reach the point of being exhausted. |
 |
Activity Levels
Keeping track of intentional and unintentional (such as walks with friends, housework, gardening, unexpected stairs) exercise helps paint a picture of your day-to-day activity levels. You can use the simple activity log provided by CCI, or if you have a fitness tracker you can make sure this is recording activity. |
 |
Sleep Patterns
Sleep is crucial for everyone, but a lot of the time we are unaware of our sleep patterns. Tracking what you do before bed, the time you go to sleep, how often you wake up, your total hours of sleep and how you feel of a morning can help draw connections with fatigue. You can use the free sleep diary or log provided by the Sleep Foundation. |
ACTIVITY: Monitor for 1 week
Using the templates provided in the Valion Fatigue Diary, or your own, monitor your fatigue, sleep and activity over the course of one week. Bring this to your next session to discuss with your doctor or Valion team member. Together you can identify potential links and develop a plan to conserve energy.
TIPS: Managing Fatigue
Firstly, it is important to remember that the goal here isn’t to create the same energy levels you had prior to your cancer diagnosis. The key focus of managing fatigue is finding ways to conserve energy and mitigate factors (where possible) that could be contributing to fatigue.
The Three “P”s
Nothing beats alliteration for ease of remembering a simple yet effective strategy we like to call the three Ps.
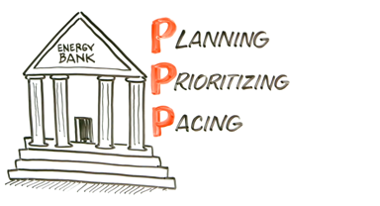
Plan: Write down all the tasks/ activities that you want to complete for the day. Include all tasks (even if you think they aren’t relevant).
Prioritise: Reorder the list based on what is most important to you (this could be related to enjoyment, urgency, sense of wellbeing, connectedness etc). Prioritising tasks ensures that the most important jobs get done before running out of time or energy.
Pace: Minimise the amount of high intensity activities done in one day. Remove anything that isn’t necessary or that can be delegated to someone else.
When looking at your list and completing the three “P”s, ask yourself the below questions to help:
- Is this necessary?
- Is it worth using that much energy? What might I miss out on if I do this?
- What if the task was not done?
- How else can this be achieved?
- When is the best time of day to complete this task?
ACTIVITY: Do your first “3 P” in session
 |
At your next session with your clinician, work together to complete the three “P”s for the day ahead or the next day (depending on what time your session is). It can be helpful to have guidance and input when doing your first planning, prioritising and pacing of activities. It can also keep you accountable! |
Fuel your body
Food is a key source of energy that is crucial for managing fatigue. Below are some simple steps you can take to ensure you are getting adequate nutrition to support energy levels.
- Keep your tank topped up across the day. If you are having trouble with your appetite, aim to eat small meals or snacks instead of larger meals.
- Ensure an adequate intake of key food groups across the day; protein (important to eat enough and dose protein regularly throughout the day into all meals and where possible snacks), dairy (high in calcium & protein), grains (high in fibre), vegetables, fruit, health fats including omega 3’s which can help with some of the inflammatory causes of fatigue. Refer to the Cancer Council Nutrition Booklet for nutrition advice and meal ideas.
- Take snacks to appointments and keep in the car in case of delays.
- Keep it simple. Meal prep and freeze for days where you don’t have the energy to cook, utilise online shopping avenues, sign up to a meal delivery service.
- Check with your health professional team before starting nutrition supplements.
Be Active
It used to be thought that ‘rest was best’. But, it’s important to know that appropriate exercise has been shown to be safe for people with cancer-related fatigue, and one of the best ‘treatments’ to improve energy levels and reduce fatigue levels. What type of exercise, for how long and what “intensity” (how hard you push) is all individual. Most people find a 10-15 minute walk at a moderate pace each day is a good place to start, and build up from there. If you have just had a chemotherapy infusion usually the 3-4 days after is the hardest to be active, but even a walk to the letterbox and back a few times a day is a great pace to start. Speak with an Accredited Exercise Physiologist or Physiotherapist with experience in cancer support for specific advice.
Support your mind
Experiencing fatigue can be stressful. Its impacts on your life can increase feelings of hopelessness, which can impact your overall mental wellbeing. Many people with cancer benefit from seeing a psychologist. It can help with managing stress associated with fatigue, assertive communication, addressing unhelpful thought patterns, overcoming barriers to exercise and relationship tension.
Remember, even though you might feel alone in your diagnosis of cancer, it doesn’t mean you should tackle its impacts alone. Getting support can help charge your battery! If seeing a psychologist interests you, chat with your health professional team to arrange a referral.
Key Takeaways
Resources and Further Reading
Below are some useful resources (some mentioned throughout this module) to help monitor and manage cancer-related fatigue.
If you would like to know more about cancer-related fatigue, below are some recommended articles and videos. If you have any questions, be sure to write them down and bring them to your next session.
| Dealing with Cancer Related Fatigue
Peter Mac & Australian Cancer Survivorship Centre. |
|
| Understanding Cancer Related Fatigue
Dr Mike Evans |
|
| Exercise and Fatigue
Learn from Valion Exercise Physiologist Emma |
|