There’s nothing better than feeling a sense of wellbeing in both your mind and body. Yet, we are only in the early stages of understanding how this often ‘tenuous’ balance between mental and physical health is achieved.
It’s clear that an illness or physical health condition often contributes to a change in our mental wellbeing. We also understand that the interrelationships between how our mind and body respond to illness are complex, extending beyond the impact of not being able to do what we want, or the pain and suffering caused by disease.
The impact of long COVID is one example of the suspected link between the development of depression and anxiety, following infection, that we think may lead to brain changes. In addition, a recent article in The Guardian covered a study in the UK showing a link between depression and the development of type 2 diabetes and evidence supporting the connection between mental health and gut health is steadily mounting up.
But what about when we are experiencing physical health symptoms that do not have an underlying ‘physical cause’. This can be a much more difficult to understand.
This week, in the lead up to RU OK Day, Valion Health Clinical Psychologist Rebecca Van Lloy, took some time to talk to us about the interconnectedness of mental health and physical health and how a significant change in your physical health may point to underlying changes in your mental health such as the onset of depression or anxiety.
What does it mean if the doctor doesn’t find ‘anything ‘wrong’?
Rebecca says there are a range of symptoms that lead people to their doctor, that may be linked to mental health. These include:
- headaches
- low blood pressure
- body aches
- muscle weakness
- persistent fatigue
- digestive problems
- brain fog
- waking feeling unrefreshed
- an increase or decrease in appetite and/or sudden weight changes.
Rebecca says sometimes the stigma attached to mental health means people look for a solution to their physical ailments before considering their mental health.
“When screening and bloodwork don’t reveal a physical illness and people are experiencing chronic pain or neurological symptoms, they may not feel believed or that their physical symptoms are real.
“We know that these physical symptoms are very real, that they impact a person’s quality of life and can be debilitating. Unravelling the complex interplay between mental and physical is a key focus of how we now think about and approach mental health,” she says.
What we know now, is that strategies to improve mental health usually result in physical gains and improvements in physical health often yield mental health gains.
But it can be difficult for people to recognise this relationship especially if they are used to experiencing ‘good mental health’ or if there is no obvious ‘triggering event’ or cause.
Rebecca says the relationship between physical health and mental health often starts with the impact of hidden stress.
“It is important to stay tuned in to what is going on with your physical health as it can be a useful indicator of a change or decline in your mental health, before you even recognise you have shifted from thriving to surviving.”
Good mental health means you can deal with stress, and remain focused, flexible and productive in difficult times as well as good times. It influences how you think, feel and act and helps you make choices that match up with what matters the most to you.
“When you have good mental health, you don’t need to rely on salt and sugar to manage low energy, you don’t need to binge watch TV to recover from a stressful day, retreat from others to cope, or have that glass of wine instead of going for a short walk at the end of your day,” says Rebecca.
Mental health is for everyone
First up, it’s helpful to know that good mental health is more than just the absence of stress, or a mental health diagnosis. The World Health Organization says:
Mental health is a state of mental well-being that enables people to cope with the stresses of life, realise their abilities, learn well and work well, and contribute to their community. It is an integral component of health and well-being that underpins our individual and collective abilities to make decisions, build relationships and shape the world we live in
Another helpful point to know is that mental health is a continuum and it’s perfectly normal for people to experience ebbs and flows in their ‘headspace’ as they go about daily life.
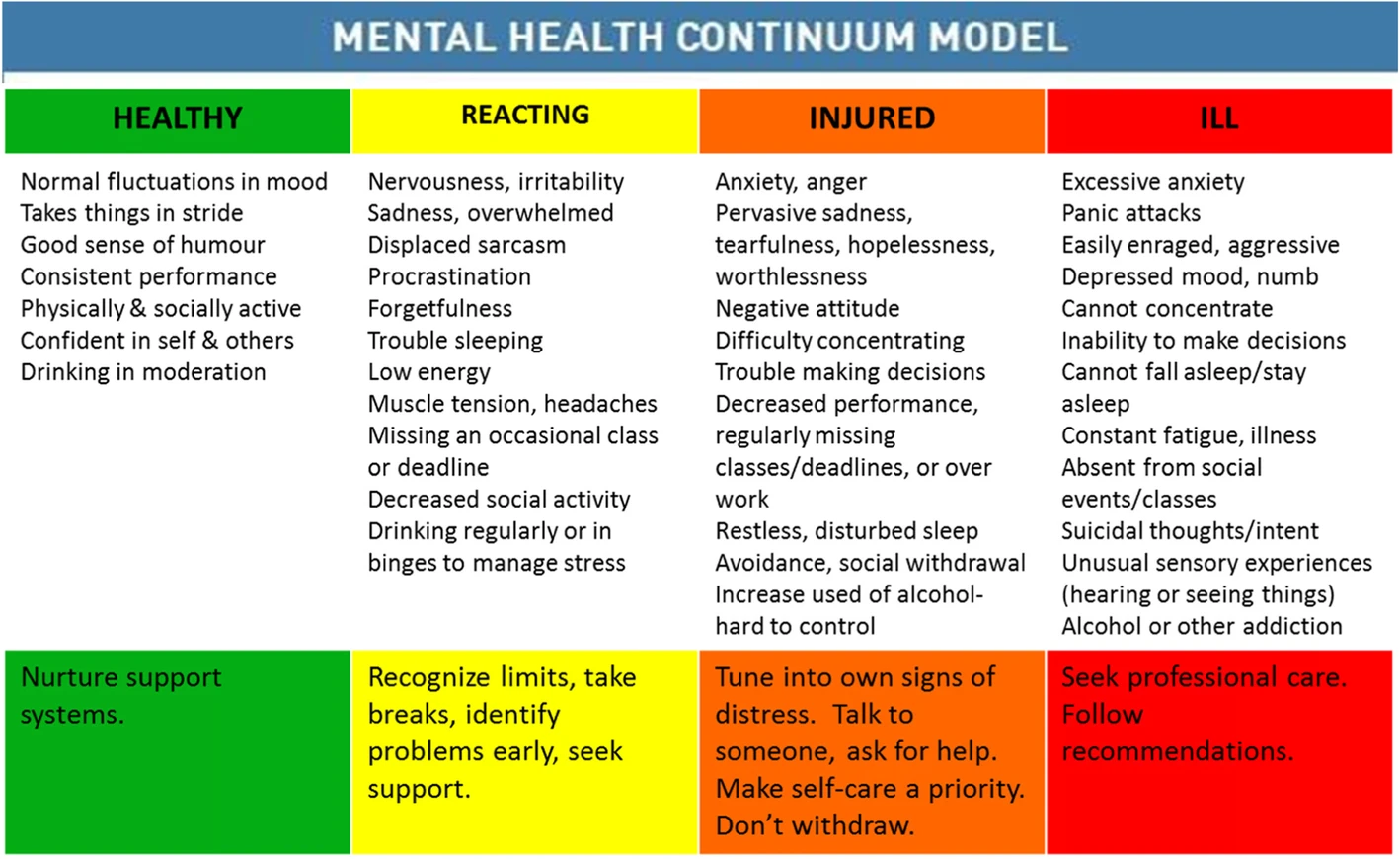
Mental Health Continuum Model (Image Source: Canadian Armed Forces)
Rebecca says the mental health continuum is a tool which can help us think about our wellbeing and what actions we can take to improve it. It helps us to identify if our mental health is low and when we might need more support.
Exercise as medicine? Eating for depression?
Good mental health makes it easier to maintain a balanced lifestyle and engage in behaviours that support physical health, but how do we achieve this if we are already struggling or operating in survival mode?
Unsurprisingly, the best ways to support mental health to improve physical health, and vice versa, are to stay connected, keep exercising, sleep well and eat well.
Rebecca says there’s a lot of research linking the relationship between our diet, immune activation and our mental health, and she says there are clear links between what we eat and how we feel.
In addition to diet, your GP or health practitioner is also likely to talk to you about the role of exercise as an important tool in the prevention, treatment and rehabilitation of a range of illnesses.
A new study by the University of South Australia recently showed that physical exercise is 1.5 times more effective for managing mental health than counselling or the leading medications and researchers are calling for exercise to be a mainstay for managing depression.
We all know this stuff works, but it sometimes feels impossibly hard to make the right choices.
Rebecca says, that while this research is exciting and important, it can be tricky for people who are struggling with fatigue, low energy, loss of motivation or feelings of anxiety to make the changes they know are good for them.
According to Rebecca, problems with motivation and decision making can also feel completely overwhelming for people struggling with stress, anxiety and depression.
“The basics seem insurmountable, and people may experience a cycle of indecision and guilt as they struggle to get the day started or get caught up ‘should-ing themselves’ all day –‘I should really go for a walk, I should call my doctor and make an appointment’.
“People sometimes need a lot of support and encouragement to make these kinds of changes. Overcoming the ‘mental hurdle’ of getting started can be a genuine obstacle.”
Starting small
Rebecca says taking small, sustainable steps is the most effective way to overcome the mountain in the mind.
“Start small and be consistent,” she advises. “We tend to think about exercise or activity as big actions like a 30-40 min walk or catching up with a friend for an hour.
“But in reality, maintaining the smallest level of activity to ‘keep moving’ and ‘keep connected’, whether it be a 5-minute walk or a 5-minute phone call, is fine.”
If you notice you don’t ‘feel like yourself’ and you suspect your mental health could be impacting your physical health, the best place to start is your doctor. Your GP can ensure that they have considered any other reasons that might explain your physical symptoms and also discuss formal and informal ways to scaffold your mental health.
It might be starting with a formal referral for exercise or a psychologist, or even a social prescription to an activity, group in your local area that helps you get moving and stay connected.
Rebecca says initiatives like Valion Health’s, Health Coaching Programs also actively support people to re-establish or start working on their physical health and connect them expert mental health professionals and allied health support.
Actions for RU OK Day and beyond
R U OK Day is a reminder to check in on anyone you think might be struggling with their mental health. Rebecca says it’s helpful to:
- Avoid advice giving:
Instead of saying: ‘you should go for a walk, it might make you feel better’, it’s better to grab the car keys and say: ‘hey feel like going to the park and sitting in the sun with me for 15 minutes.’
- Validate physical and mental symptoms:
People feel better when they feel understood so instead of taking a mind over matter approach it’s important to acknowledge their experience and how difficult it can be to achieve even the simplest activity. Try saying: ‘I know you have no energy to go out right now, how about I come over with a smoothy and a healthy lunch and we hang out for half an hour’.
Learn more about RU OK Day here.
Mental Health Coaching with Valion Health
Our Mental Health Coaching program is for participants who are at risk of, or who have a mental health condition and require support. Together with a primary mental health professional we will help you recover and reach your health and wellbeing goals.
Valion Health conducts Mental Health Coaching by phone and videocall and offers participants high quality, personalised mental health care and support from the comfort of their own home.
Our Mental Health Coaching program will help you:
- Increase your confidence and motivation to change unhealthy behaviours
- Identify and build on supportive behaviours that benefit your mental health
- Increase your knowledge and understanding of mental health conditions
- Offer proactive strategies for managing mental health and how to implement these day-to-day.
Learn more about Mental Health Coaching and whether you are eligible.